A transient ischemic attack or TIA (also known as a mini-stroke) is the same as a stroke, except that the symptoms last for a short amount of time. This guide explains what the symptoms are, what you should do if you have them and how a TIA is diagnosed and treated.
What is a TIA?
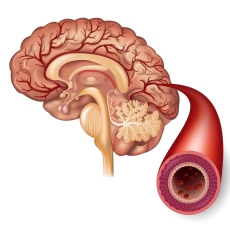
A TIA is the same as a stroke, except that symptoms only last for a short amount of time. In a TIA, a blood vessel in the brain gets blocked, but the blockage clears by itself. TIA is also known as a mini-stroke and some people think of it as a ‘funny turn’. But a TIA is a major warning sign of a stroke.
Spotting the signs of a stroke
The FAST test (left) helps to spot the three most common signs of stroke or TIA. But there are others that you should always take seriously. These include:
• sudden weakness or numbness on one side of the body, including legs, hands or feet
• difficulty finding words or speaking in clear sentences
• sudden blurred vision or loss of sight or in one or both eyes
• sudden memory loss or confusion, and dizziness or a sudden fall
• a sudden, severe headache. Stroke can happen to anyone, at any age.
Every second counts. If you spot any of these signs of a stroke, don’t wait. Call 911 straight away. There is no way of knowing whether you are having a TIA or a full stroke when the symptoms first start. If you, or someone else, show any of the signs of stroke or TIA you must call 911.
FAST test:
• Face Can the person smile? Has their face fallen on one side?
• Arms Can the person raise both arms and keep them there?
• Speech Can the person speak clearly and understand what you say? Is their speech slurred?
• Time If you see any of these three signs, it’s time to call 911.
Some of these symptoms can be caused by other things such as low blood sugar, a migraine, an inner ear problem or a seizure. However, you cannot be sure of the cause until your symptoms are investigated by a doctor.
What causes a TIA?
Like a stroke, a TIA is caused by a blockage cutting off the blood supply to part of your brain. The only difference when you have a TIA is that the blockage is temporary – it either dissolves on its own or moves, so that the blood supply returns to normal and your symptoms disappear. The blockage is usually a blood clot, although rarely it can be caused by other things, such as a piece of fatty debris or an air bubble in your blood stream. Blood clots may form in areas where your arteries have become narrowed or ‘furred up’ by fatty deposits. This process is called atherosclerosis. If you have a heart condition, such as atrial fibrillation, blood clots can form in the heart and move up into your brain. Some strokes and TIAs are caused by small vessel disease, which involves damage to the tiny blood vessels within the brain. Deposits collect in the blood vessels, causing them to thicken. If they become completely blocked, this can lead to a stroke or TIA.
Symptoms of a TIA
These can sometimes be caused by bleeding in your brain (called a hemorrhage), but this is unusual. Sometimes people have a TIA that affects their vision. This can happen when a blood vessel leading directly to your eye becomes blocked and causes a temporary loss of vision. This is sometimes called amaurosis fugax or transient monocular blindness. People often describe it as feeling like a curtain has fallen over one eye. It can also happen when the visual parts of your brain are affected, leading to vision loss in one or both eyes, or on one side, or double vision.
How is a TIA diagnosed and treated?
Initial assessment A TIA is diagnosed with a medical examination, and in many cases a brain scan. Reasons why you might be offered a brain scan include:
• it is suspected that the TIA is caused by a hemorrhage
• the doctor needs to determine the position of the TIA in the brain
• the symptoms have been prolonged and therefore a stroke rather than TIA is suspected
• another cause for your symptoms other than TIA is suspected
• you are taking anticoagulants.
If you have a suspected TIA you should either be referred straight away to your primary care physician or an emergency room. In most cases you should see a stroke specialist within 24 hours. Everyone who has a TIA is at an increased risk of stroke, so it’s important to ask your doctor to explain your own risk, and what you should do to reduce it. As many as four out of five strokes can be prevented after TIA if the correct tests and treatments are carried out.
Treatments to reduce your risk
It is likely that the doctor will give you aspirin to take until you see a stroke specialist. This will help to prevent blood clots forming.
Assessment with a specialist
Usually you will be referred to a consultant neurologist (a doctor who specializes in conditions that affect the brain and spine), or a consultant stroke specialist for further assessment. If the specialist suspects that you have had a TIA or perhaps that your symptoms are caused by something else he or she may want you to have a brain scan. You will either have a computed tomography (CT) scan or a magnetic resonance imaging (MRI) scan. Both of these produce pictures of your brain and will help doctors to rule out other causes of your symptoms. You may also be offered some of the following tests and checks:
• electrocardiogram (ECG): checks the heartbeat
• Doppler ultrasound: checks for blockages and narrowing of the neck arteries
• blood pressure measurement.
Your blood will be checked for:
• blood clotting
• blood sugar
• cholesterol levels.
If you are diagnosed with a TIA your specialist should talk to you about the factors that are increasing your risk of stroke and what you can do about them. This may mean taking medication or making changes to your lifestyle, such as stopping smoking, exercising more and drinking less alcohol, or both. In some clinics you may also see a clinical nurse specialist who can give you further advice. You should be offered a follow-up assessment if you need it.
What impact will this have on my life? Although the physical symptoms usually disappear quickly, the impact of a TIA can last much longer. With the right treatment you should start to feel back to normal quickly and you won’t have any lasting effects. If you do notice ongoing problems, such as muscle weakness or effects on your memory, understanding or speech, you need to go to your GP.
You should be given advice about other ways of reducing your risk of another TIA or stroke. Some people need to lose weight, exercise more, give up smoking or drink less alcohol. All of these actions can also help to manage other health conditions and will often make you feel better. If you have any questions or concerns about your medication, go back to your doctor or pharmacist and ask. Tell them if you are worried about side effects, as there will often be an alternative that you can take. Never stop taking your medication without talking to your doctor first. Many people consider having a TIA as a ‘wake-up call’ and a sign that they need to make some lasting changes to their lifestyle. Remember… A TIA is the same as a stroke, except that the symptoms last for a short amount of time. Just like a stroke, a TIA is a medical emergency.